Vaginal Dryness During Menopause: Why You Don’t Need to Suffer in Silence
- Dr. Emily Hartman

- Oct 27, 2025
- 4 min read
Updated: Dec 14, 2025

Let's be honest. Of all the possible symptoms of perimenopause and menopause—hot flashes, night sweats, mood swings—vaginal dryness is often the one we’re least likely to discuss, even with our closest friends. It can feel embarrassing, private, and maybe even a little "shameful," as if it's a personal failing.
Many of us just accept it as an inevitable part of aging, something to be quietly endured. But here’s the truth: You absolutely do not need to suffer in silence.
Vaginal dryness, and the discomfort that comes with it, is an incredibly common and incredibly treatable medical symptom. It's not a personal failure; it's a physical change with real, practical solutions. Thinking of this as just another manageable symptom, like needing reading glasses, can help change the entire conversation.
What’s Really Going On? (It’s Not Just "Dryness")
That feeling of dryness, itching, or burning isn't in your head. It’s the direct result of hormonal changes.
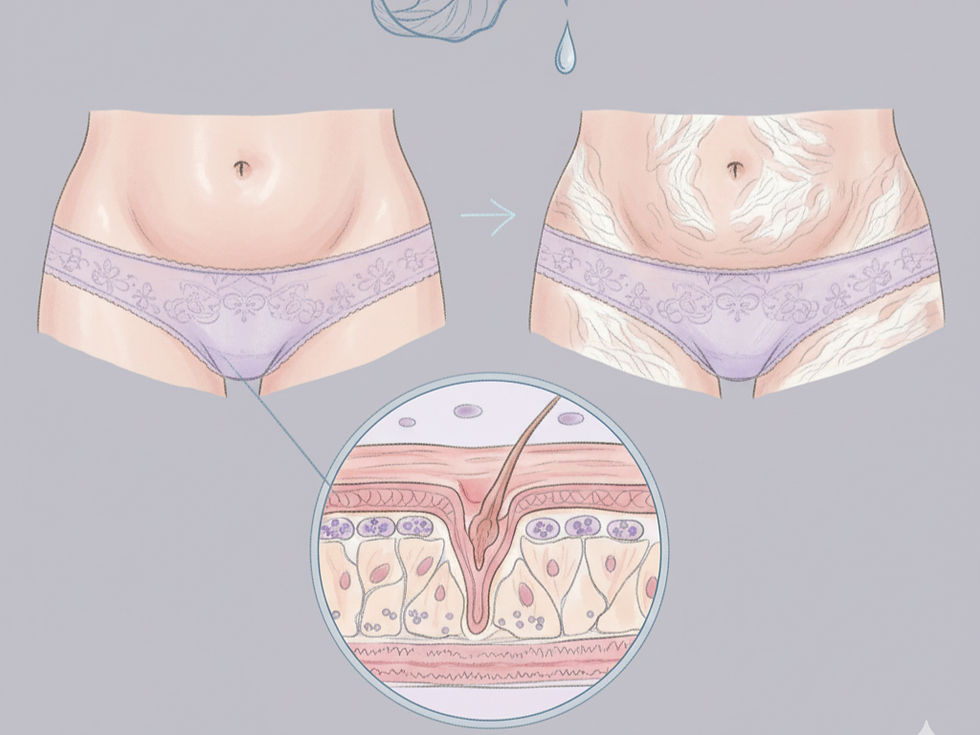
Here’s the simple version: The hormone estrogen acts as your body's natural "plumping and moisturizing" agent for vaginal tissues. It keeps the vaginal lining thick, elastic, and well-lubricated. As you enter perimenopause and menopause, your estrogen levels naturally decline.
Without as much estrogen, those tissues can become:
Thinner
Drier
Less elastic
More fragile
This is why "vaginal dryness" is actually an incomplete term. Your doctor or a specialist from the North American Menopause Society (NAMS) will likely call it Genitourinary Syndrome of Menopause (GSM).
That’s a medical-sounding name, but it's important because it covers the full picture of what you might be feeling. GSM includes a whole cluster of symptoms that can affect both your vaginal and urinary health:
Vaginal Symptoms: Dryness, burning, itching, and general irritation.
Urinary Symptoms: Feeling like you have to "go" all the time (urgency), needing to go more often (frequency), or even experiencing more urinary tract infections (UTIs).
Symptoms with Intimacy: Pain during sex (this has its own medical term: dyspareunia). This isn't just a "lack of libido"—it's actual physical pain caused by friction and fragile tissues.
You are not alone in this. NAMS reports that as many as 50% of postmenopausal women in the US experience symptoms of GSM, but sadly, only a small fraction of them seek treatment.
Starting with Simple Steps: Moisturizers vs. Lubricants
Before jumping to prescriptions, many women find relief with over-the-counter (OTC) products. The key is knowing what to buy, because moisturizers and lubricants do two very different jobs.
Vaginal Moisturizers (For Daily Comfort)
Think of these like a high-quality, long-lasting moisturizer for your face. You don't just put it on when your skin feels dry; you use it regularly to maintain skin health.
What they do: These are designed to be used 2-3 times a week (not just during sex). They absorb into the tissue to hydrate it, helping to restore moisture and improve comfort on a daily basis.
What to look for: Look for products that are specifically formulated for vaginal use. You want them to be free of parabens, glycerin, perfumes, or hormones. Many contain hyaluronic acid, which is excellent at drawing moisture into the tissues.
Vaginal Lubricants (For Intimacy)
These are your "in the moment" solution. Think of them as helping with friction when you need it.
What they do: Lubricants are used during sexual activity to reduce friction and make intimacy more comfortable and pleasurable. They don't fix the underlying dryness, but they make the experience better.
What to look for: Water-based or silicone-based lubricants are your best friends.
What to avoid: Do not use Vaseline (petroleum jelly) or any oil-based products (like baby oil or coconut oil) internally. They can trap bacteria (increasing infection risk) and can damage latex condoms.
Key takeaway: For many women, the best approach is using both—a regular moisturizer for overall tissue health and a lubricant for comfort during sex.
When OTC Isn't Enough: Real Medical Solutions
Here is the most important message you need to hear: If OTC products aren't cutting it, you are not out of options. You have simply reached the point where you need a solution that restores the tissue, not just covers up the symptoms.
This is where you talk to your gynecologist or primary care provider (PCP). The "gold standard" for treating GSM is replacing the estrogen that's missing—but only in the area that needs it.
Local Estrogen: The Gold Standard
This is not the same as systemic hormone therapy (the pills or patches used for hot flashes).
Local, or vaginal, estrogen is an extremely low-dose treatment that works only on the vaginal and urinary tissues. It has minimal to no absorption into the rest of your bloodstream. The FDA has approved these treatments as safe and effective for this specific purpose.
Because the dose is so low, these options are considered very safe for most women, even many who can't take systemic hormones. Your doctor can help you decide.
These treatments come in a few easy-to-use, "set it and forget it" forms:
A low-dose vaginal cream. You typically use a small applicator a few times a week.
A tiny vaginal tablet. You insert this with a disposable applicator, and it dissolves.
A soft, flexible ring. Your doctor places this in the vagina, and it slowly releases a very low dose of estrogen over three months. You don't feel it, and it can stay in during sex.
Other Prescription Options
If you and your doctor decide local estrogen isn't the right fit for you, that doesn't mean you're out of options. There are other FDA-approved, non-estrogen prescription treatments available. These can come in different forms, such as a daily pill or another type of vaginal suppository, that work in different ways to help relieve symptoms.
The point is: You have choices. Don't be discouraged if the first thing you try isn't the perfect solution.
Conclusion: Relief Is Possible (and You Deserve It)
This new chapter of life is about finding new ways to thrive. Dealing with vaginal dryness, or GSM, is not a sign of defeat—it's just a new item on your self-care checklist.
It’s an incredibly common, shared experience among women. And thankfully, it's one of the most treatable symptoms of menopause. Whether you find relief with a simple over-the-counter moisturizer or by talking to your doctor about safe, local, and effective prescription options, the most important step is the first one: Acknowledging that you don't have to just live with it.


Comments